Background:
Diffuse large B-cell lymphoma (DLBCL) represents the most prevalent subtype of non-Hodgkin lymphoma. Despite advancements in treatment, the prognosis for relapsed and/or refractory DLBCL (R/R DLBCL) patients remains unfavorable due to the development of drug resistance and disease progression. The pressing need to enhance the outcomes in R/R DLBCL patients necessitates ongoing investigations into novel therapeutic approaches. Among various exportins, the nuclear export protein exportin 1 (XPO1) solely governs the transportation of nuclear proteins harboring leucine-rich hydrophobic nuclear export signals (NES), including essential regulators like p53, RB1, and p27. Selinexor, an oral inhibitor specifically targeting XPO1, has emerged as a promising candidate in R/R DLBCL patients. Encouraging findings from a phase II clinical trial demonstrate a more favorable efficacy of Selinexor in the germinal center B-cell (GCB) subtype compared with that in other subtypes of DLBCL. Nonetheless, the clinical implementation of Selinexor has led to the emergence of acquired resistance, posing a significant challenge for medical practitioners. Efforts to overcome this resistance and establish strategies to maximize Selinexor's therapeutic potential remain of paramount importance in addressing the urgent clinical needs of R/R DLBCL patients.
Methods:
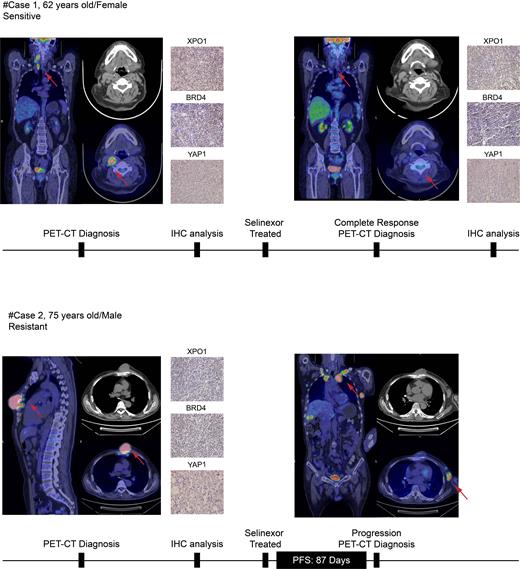
Characterization of Selinexor resistance targets was performed using a CRISPR/Cas9 screen transcription factors library pool at 0-day and 14-day time points after treatment. Cell function experiments in vitro were applied to verify the screening results and therapeutic efficacy was tested in vivo in NSG mice. Synergistic treatment approach utilizing BRD4 inhibitor JQ1, known for its curative effects in AML, MM, and ALL, in combination with Selinexor were also evaluated. Mechanistic exploration of BRD4's role in Selinexor resistance was further analyzed via RNA-seq, ChIP-seq, as well as luciferase reporter experiments. Therapeutic outcomes were evaluated in R/R DLBCL patients undergoing Selinexor treatment via PET/CT imaging.
Results :
BRD4, BRD7, ZMYND8, and YTHDC1 were identified as top Selinexor resistance candidate targets through CRISPR/Cas9 Screen. The knock-down of BRD4 enhanced the killing ability of Selinexor in vitro and reduced tumor burden in subcutaneously transplanted tumor mice after treatment with Selinexor in vivo in DLBCL. The combined treatment with BRD4 inhibitor JQ1 and Selinexor had a stronger ability to promote cell apoptosis, enhance DNA damage and reduce nascent DNA compared with the single drug group. Hematological and organ toxicity tests confirmed an acceptable toxicity for the combined drug regimen. ChIP-seq differential peaks and RNA-seq differential genes analysis elucidated the crucial role of YAP1's sub-cellular localization under Selinexor treatment. YAP1 nuclear translocation enhanced transcription and formed an interaction with BRD4, resulting in augmented BRD4 binding domain, and finally lead to the resistance of Selinexor. PET/CT imaging showed that one patient with high XPO1 expression achieved complete response (CR), exhibiting a sensitivity to Selinexor treatment, but the other exhibits resistance associated with a lack of XPO1 expression and BRD4-regulated acetylation.
Conclusions:
The nuclear translocation of YAP1 and its interaction with BRD4 mediated the transcriptional regulation and further induced resistance to Selinexor in DLBCL. BRD4 inhibitor JQ1 combined with low-dose Selinexor can mitigate blood toxicity and enhance therapeutic efficacy, achieving an improved outcome.
Disclosures
No relevant conflicts of interest to declare.